
Dan O'Neill
@dp_oneill
Healthcare services, tech & policy nerd. Alum: @theNAMedicine, @StanfordEng, @SAISHopkins, @CMCnews, @BCG and various health services & tech cos. Views my own.
In @nejmcatalyst, @ALKaplan_MD and I tackle the #Covid shock to hospital & physician practice finances. As Warren Buffett says, "when the tide goes out, you find out who's been swimming naked" Or, in this case, who has bet heavily that prices & volumes will only ever go up. 1/n
The Covid-19 pandemic has highlighted the urgent need for health care providers to abandon volume-based payments in favor of models that give them financial stability in volatile times. catalyst.nejm.org/doi/full/10.10… #COVID19 #SARSCoV2
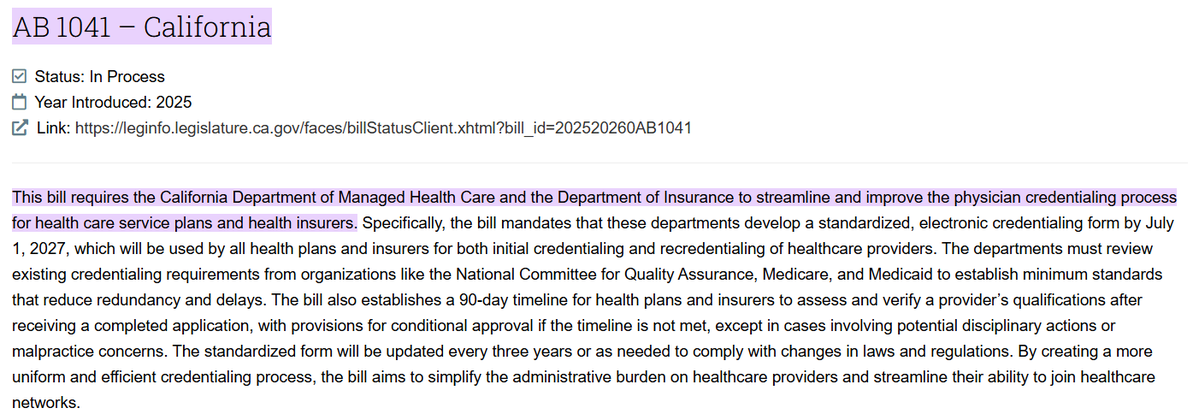
A proposed bill in CA sets a 90-day clock on insurers' provider credentialing processes. Two surprising things: 1) That payers need a directive to improve their own administrative inefficiency 2) Despite the low bar (it could be entirely automated), this might actually help!
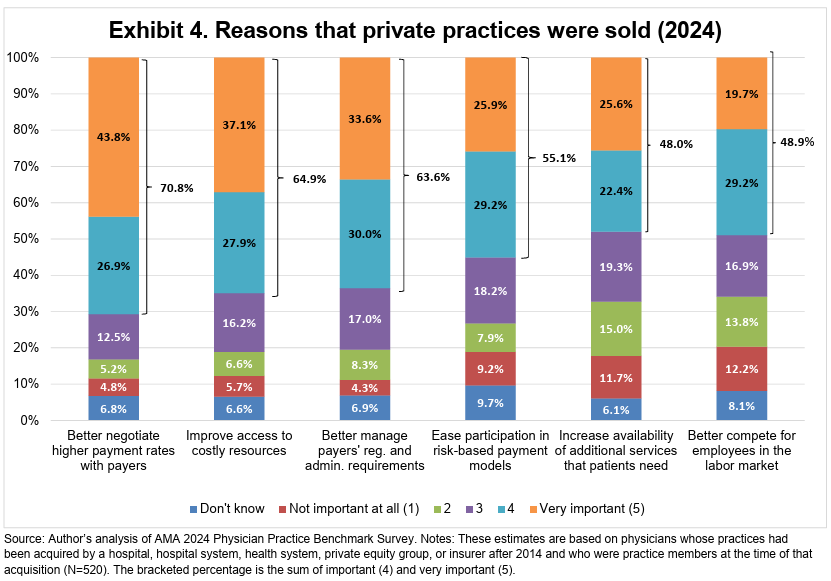
Pretty clear example of how selective contracting in healthcare drives consolidation, which boosts prices, which then begets more consolidation…
Third, physicians bought by hospitals with more bargaining power experienced larger increases in prices.
We show evidence that physician AND hospital prices go up. Physicians that got acquired saw price increases of 15%. Hospital prices went up by about 3%.
This seems like a genuinely useful step. Tip of the hat to @Humana. Now, if more health systems let patients connect records from different MyChart accounts, and a few more insurers follow suit, we'll be inching toward a modern experience...
I understand that nobody wants their payment rates to decline. But is it really plausible to argue that, say, radiology reads or joint replacements have NOT become more efficient over the past 10-15 years? 🤨 statnews.com/2025/07/16/med…

The initiative to curb abusive skin substitute billing in the Medicare proposed PFS rule is highly technical, but also raises an interesting question: How does the political economy of health spending change when a large constituency of providers has an interest in lower costs?
Tech startups often gripe that healthcare providers are slow to adopt new software. But once you become a provider and have to deal with a few startup vendors’ amateurish/absent processes, disruptive changes and desperate scramble for margin… the calculus looks a bit different.
This almost certainly understates the administrative costs of the new Medicaid paperwork requirements. Dealing with that bureaucracy, and the extra coverage churn, is going to be a massive, recurring hassle for medical practices and hospitals, as well as the actual patients.
Our new analysis just up at Health Affairs Forefront: we project administrative costs stemming from national Medicaid Work Requirements as in the "Big Beautiful Bill." We estimate: > $5 billion in new administrative costs, equal to > $950 per beneficiary dis-enrolled, or
It has been interesting to see One Medical caught up in this contract fight between Blue Shield and the University of California medical centers. Ultimately a revealing look at One Med’s business model - i.e. how and why their rates are often unusually high.
UC Health and Blue Shield of California on Monday extended contract talks to Aug. 9, giving thousands of patients more time before possible care changes. sfchronicle.com/health/article…
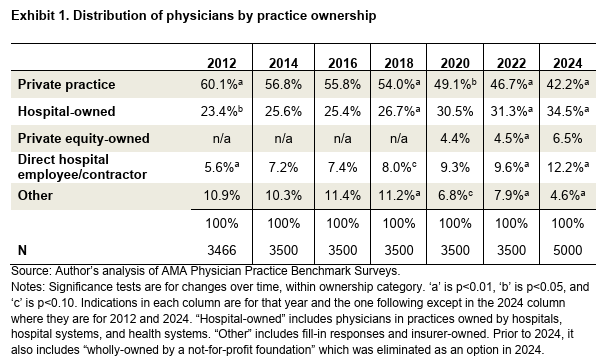
Helpful data on medical practice ownership. As shown elsewhere, hospital buyouts are a much bigger factor in consolidation, and the recent↗️in consolidation, than is private equity. And if insurers want a competitive provider landscape, they have to stop strangling independents
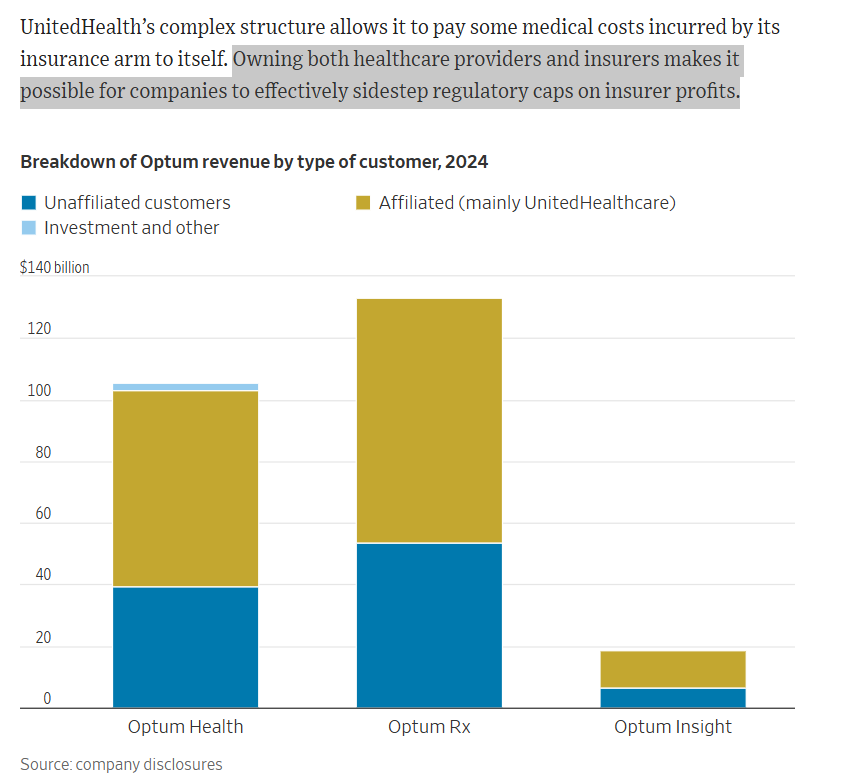
Pretty clear @WSJ summary of concerns about vertically-integrated insurers (not just UHC!). The "provider" subsidiaries do depend on the parent insurer steering patients their way. And, what's not mentioned - the insurer obligating independent providers to contract with that sub
Interesting study, suggesting that employers in Colorado mountain towns lowered premiums by 13-17% by collectively negotiating lower provider prices. Perhaps a bit like Germany, which has private providers & plans but uniform regional fee schedules. onlinelibrary.wiley.com/doi/10.1111/jo…
One way to look at societal affordability in healthcare? We made real headway on Medicare in the post-ACA decade (and a half)… …but we’ve made little or no progress for the majority of Americans and all the employers & entrepreneurs not protected by Medicare or Medicaid.
A humble suggestion: How about we work to make American health care affordable again? Right now, the focus is just the opposite. jamanetwork.com/journals/jama-…
Using MA claims/Star rating data for 872 PCPs in 7 states who took on full risk for their MA patients, we found women PCPs had better quality outcomes and their patients had fewer ED visits and hospitalizations. Women earned the same per patient under FFS and *MORE* under VBP.